For Medicaid Plans
Improving outcomes for Medicaid members
The Wellth platform is tailored to address these challenges while motivating daily action for sustainable healthy habits.


The Wellth platform is easy to implement—from the backend technology to onboarding your members. Our programs are fully operational at scale and customizable to meet the needs of your Medicaid plan goals.
Improved health outcomes and cost savings don't have to be mutually exclusive. Learn how our partners are achieving both—with Wellth!








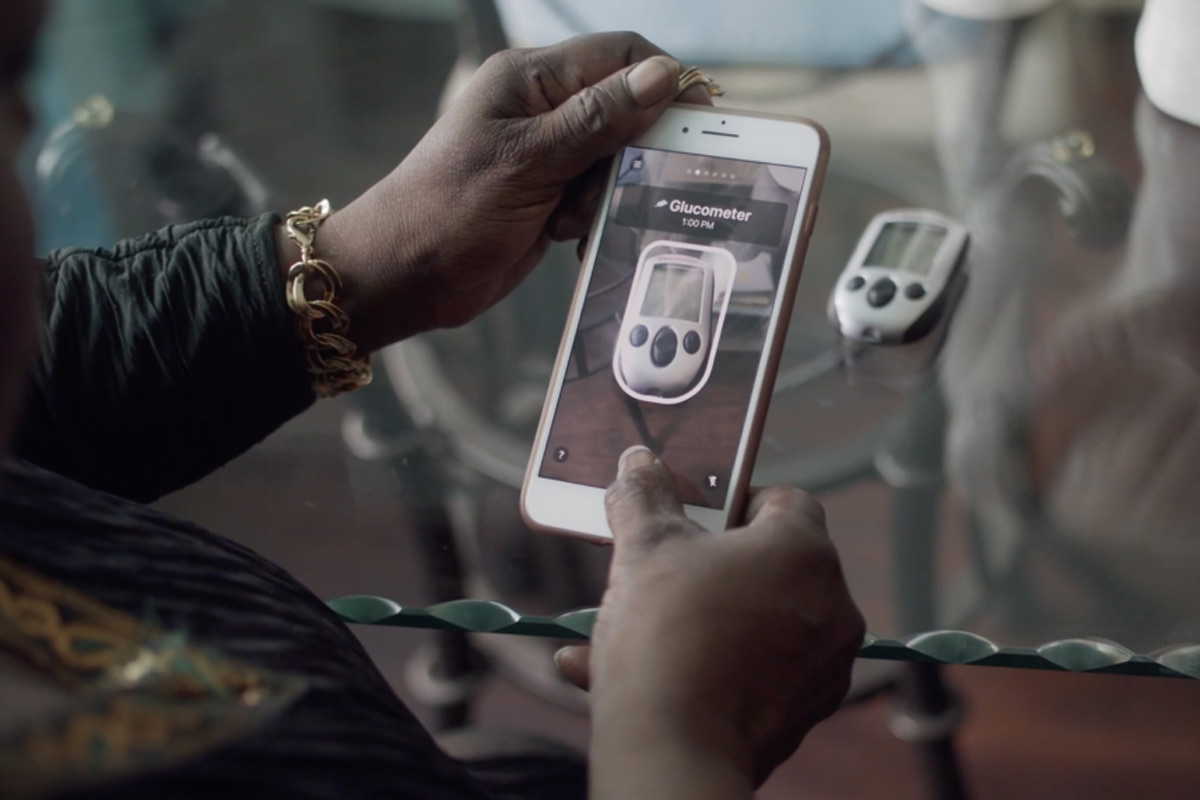

Wellth utilizes existing technology—i.e., the simple smartphone—to work within existing workflows, reducing the need for complex training or expenses. Implementation can be completed in as little as 30 days, requiring minimal lift from our partners and their IT teams.

There's nothing better than hearing how Wellth has positively impacted a person's life. It's what motivates us to bring our very best to our partners and our members!